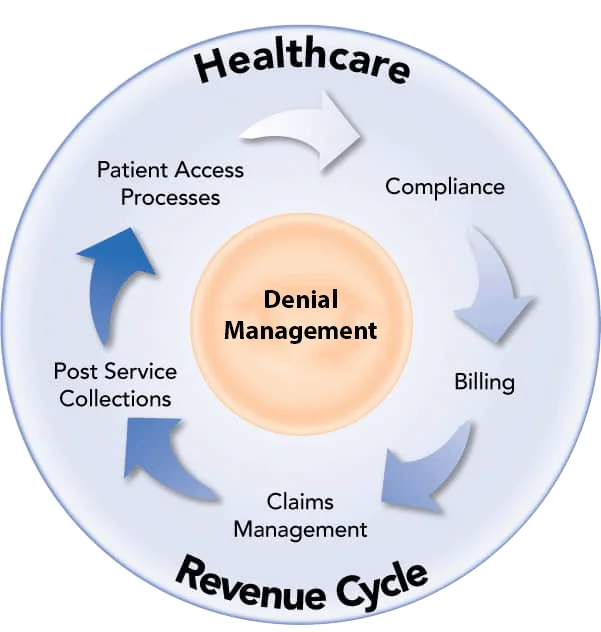
Effective management of claim denials is a key factor in a clinic’s financial health in the healthcare industry. Denials are when an insurance company refuses to pay for services rendered more frequently than you imagine. Denial management is the method of categorizing the source of the issue of rejected or denied claims made by insurers. The most effective denial management systems will not just help health organizations recover money. Still, they can also help improve the operation, cut down on mistakes in billing, and boost the overall management of revenue cycles.
Understanding Denial Management in Healthcare
Denial management is a methodical approach to analyzing the reasons for claim denials and then resolving them with insurance companies. Denials occur when a medical claim is denied or not reimbursed for numerous reasons, such as incorrect codes, inaccessible information, or policy exclusions. Without solid denial management, healthcare facilities risk losing substantial revenue and may face operating inefficiencies.
Denial management reduces rejections, speeds up resubmissions, and ensures that claims are handled efficiently. The process helps healthcare organizations recover the lost revenue, improves compliance with payer requirements, and decreases the burden of administrative tasks.
Benefits of Denial Management
Revenue Optimization: Effective denial management assists healthcare facilities in revenue cycle optimization by decreasing denials, increasing collections rates, and maximizing reimbursement.
Operations Efficiency: Streamlining procedures for managing denials increases operations efficiency by decreasing human interventions, automating workflows, and decreasing rework for denials.
Audit Readiness and Compliance: Effective denial management procedures assure compliance with regulatory agency requirements and payer guidelines, thus reducing the possibility of audits and sanctions.
The Role of Denial Management Services in Revenue Cycle Optimization
Due to the complexity of claim processing, many healthcare providers are turning to denial management to simplify their revenue cycle process. They provide expertise in dealing with denials and resolving issues, increasing the reimbursement rate and reducing the administrative burden. A few of the advantages of outsourcing denial management are:
1. Specialist Analysis and Resolution: Expertly trained professionals recognize patterns, correct errors, and verify that claims comply with the payer’s requirements.
2. Accelerate Claim Processing: The latest technology helps track denied claims quickly, which can lead to faster resolution and faster payment.
3. Improvement in Compliance: Professional Denial Management solutions ensure compliance with constantly changing policies and regulations for insurance.
4. Improved Revenue Recovery: Resubmission strategies that are effective aid in recovering money that could otherwise be lost due to claims denials.
How Denial Management Helps Medical Organizations Run More Efficiently
A well-organized denial management system assists in identifying and fixing the underlying reasons for claims being rejected. This ensures rapid and exact payments, reduces revenue leakage, and enhances operations’ overall efficiency.
Organizations can improve their efficiency by reducing the complexity of their revenue cycle operations and focusing on denial reduction. If denial management is not managed correctly, it is time-consuming and susceptible to mistakes. By streamlining this process and concentrating on prevention more than fixing it, healthcare providers can reduce the costs of denials and boost overall effectiveness.
Conclusion
The effective management of denials in healthcare is crucial to maintaining a strong income cycle and ensuring financial stability. With a solid denial management procedure for medical billing, healthcare professionals can significantly decrease the number of claims rejected, improve cash flow, and increase overall effectiveness.